Besides the ability to diagnose Crohn's or ulcerative colitis, the new method may allow personalized treatments depending on the nature of the inflammation
When inflammatory bowel disease is suspected, patients are now forced to undergo a colonoscopy - an invasive test that requires careful preparation and is performed under anesthesia. A new method developed at the Weizmann Institute of Science in collaboration with the Sheba Medical Center (Tel Hashomer) may allow a friendlier alternative: identifying intestinal infections through a stool test. Besides the ability to diagnose diseases such as Crohn's or ulcerative colitis and track their development, the new method may allow doctors to offer patients personalized treatment depending on the nature of the inflammation. The research findings are published this week in the scientific journal good.
in the laboratory of Prof. His Itzkowitz In the department of molecular cell biology, the cells in the intestinal tissue of mice are studied in detail. When the researchers noticed in the laboratory that cells that fall out of the intestinal mucosa and are excreted in the feces, remain alive even after they have been evacuated from the body, the idea for the new diagnostic method was born. "We realized that if we test the expression of the genes in these cells in human secretions, we may be able to conclude from this about disease processes in the intestine without resorting to invasive measures," says Prof. Itzkovitz.
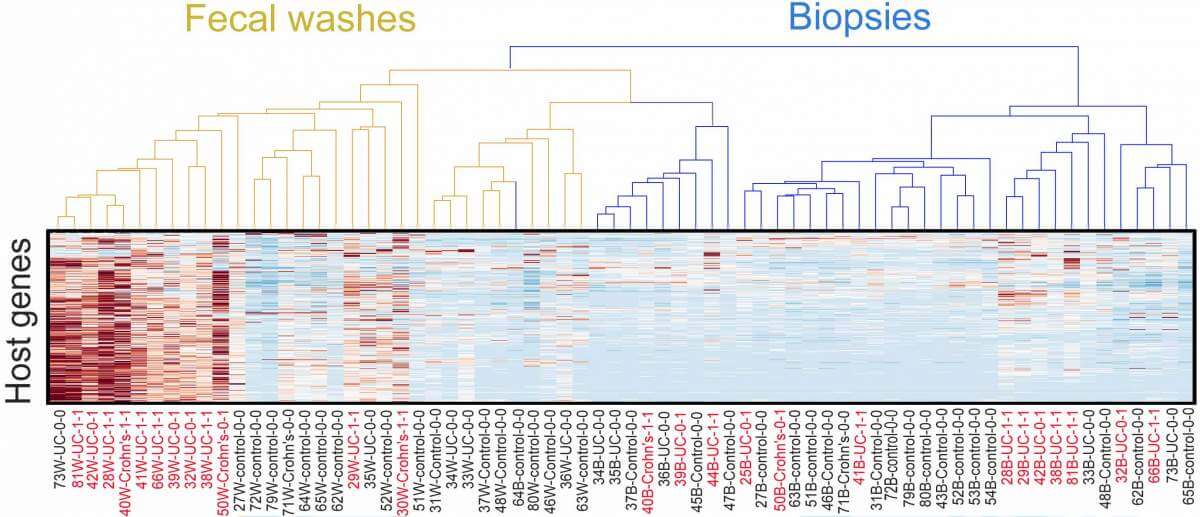
To test this hypothesis, the scientists teamed up with a team of researchers led by Dr. Bella Unger, a gastroenterologist at the Sheba Medical Center. The researchers from Sheba and the Institute examined cells of the intestinal lining taken from 30 patients with inflammatory bowel diseases who underwent colonoscopy - the origin of some of the cells was in stool samples from the colon and rectum of these patients, while the rest of the cells were sampled through a biopsy of the intestinal tissue in those areas. The researchers compared the data obtained from the patients to corresponding data from 30 healthy people who underwent colonoscopy as part of routine tests to detect cancer.
""A biopsy can miss inflammation because it provides a snapshot of the narrow piece of tissue from which it was taken, a stool sample, on the other hand, contains cells that come from all over the intestines"
To identify which types of cells were included in each of the samples, the research team used methods for sequencing the genetic material that were adapted for this purpose and other advanced methods. Besides the normal intestinal tissue cells, they also found in the stool samples four types of cells of the immune system involved in inflammatory conditions, including monocytes and regulatory T cells. With the help of algorithms developed in Prof. Itzkovitz's laboratory, the gene expression patterns that characterized the cells of the immune system in each sample were identified, and through these genetic signatures the scientists were able to determine the proportion of cells of each type in each sample - and more importantly: whether there is active inflammation in the intestine from which the cells were taken. When they compared the findings obtained from the different samples, the researchers were surprised by the clear picture that was obtained: the stool samples provided more reliable information about the presence and nature of the inflammation compared to the biopsy samples.
"A biopsy can miss inflammation because it provides a snapshot of the narrow piece of tissue from which it was taken, a stool sample, on the other hand, contains cells that come from all over the intestines," explains Prof. Itzkovitz. "A colonoscopy does indeed also include a photograph of the intestine, but there are types of inflammation that do not leave visible signs."
The information on the gene expression patterns of the cells in the stool samples may be essential not only for diagnosing intestinal infections but also for adjusting treatment for patients. Already today there are biological drugs on the market that can block in a targeted manner cells and substances that cause inflammation - instead of suppressing the entire immune system. However, these drugs only help about half of the patients and there is no way for doctors to adapt the treatment to each patient in an optimal way. Deciphering the RNA signatures that characterize the inflammation is expected to provide doctors with missing information that may make it possible to increase the effectiveness of existing treatments and possibly even develop new treatments. In addition, a quick and simple method for identifying intestinal infections will allow you to determine when treatment is necessary - and when it should be stopped.
Dr. Unger emphasizes that the new method is different from fecal tests that were developed in the past to diagnose intestinal infections, such as a test that focuses on measuring the levels of the calprotectin protein. The level of reliability of these tests, according to her, cannot replace the colonoscopy, which was and remains the ultimate test for diagnosing intestinal diseases, even though it is invasive and requires unpleasant preparations. The new method, on the other hand, is really good news, as it may allow a less invasive test, much cheaper and at least as reliable.
Also participating in the study were Miri Yabzuri, Dr. Ella Podim, Dr. Orit Pikar, Prof. Uri Kopilov, Prof. Rami Eliakim, Dr. Chen Meir, Prof. Iris Barshak and Prof. Shomron Ben-Horin from the Sheba Medical Center; Dr. Dror Shovel from the Schneider Pediatric Center in Israel; Dr. Yishai Levin and Dr. Alon Savidor from the Israeli National Center for Personalized Medicine named after Nancy and Steven Grand; and Dr. Shani Ben-Moshe, Dr. Rita Manko, Stav Dan, Adi Aguzi and Dr. Keren Behar Halpern from the department of molecular cell biology of the institute.
