Using advanced methods for genetic sequencing at the single cell level, Weizmann Institute of Science scientists reveal a new molecular mechanism of action of ketamine - and show that combining it with another drug may lead to improved performance and reduced side effects
magazine readers TEAM You were informed in July 2017 in the cover story about "New hope for depression": A low dose of ketamine, a well-known anesthetic used in operating rooms - and also in clubs as a drug for mind-altering reasons - has been identified in a series of studies as a "magic drug" for those suffering from suicidal thoughts. Two years later, in March 2019, the American Food and Drug Administration (FDA) approved the first ketamine-based depression treatment - a Johnson & Johnson nasal spray.
Although this is the most significant development in the field of depression treatment in decades, the drug is currently approved for resistant depression patients who do not respond to other treatments. The reasons for this, among others, are the fact that this is a new drug whose mechanisms of action are not yet sufficiently understood and the fear of possible side effects. In a new study published today in the scientific journal Neuron, Weizmann Institute of Science scientists reveal new details, at the level of the single cell, about the mode of action of ketamine and indicate possible directions for a safe and effective treatment of depression.
The rate of those suffering from clinical depression is constantly increasing in developed countries, including Israel; Two years of international epidemic did not help to improve the statistics. Despite the alarming numbers, the economic cost and the damage to human life, there has not been a significant breakthrough in the field of depression treatment for many decades; Certainly not since the most famous antidepressant was approved for use in 1987: Prozac. In recent years, the question marks regarding the effectiveness of the existing treatments for depression, to which a third of the patients do not respond at all, have been increasing.
Another notable disadvantage of the existing treatments is the long time it takes for them to have an effect - four to eight weeks; In patients with suicidal tendencies, such a gift is a matter of life and death. Precisely for this reason, the introduction of ketamine-based treatments is considered a breakthrough: their antidepressant effect is extremely fast - just a few hours. Moreover, the antidepressant effect continues even after the drug itself has cleared from the body. In other words, it can be said that the body's response to ketamine, more than the ketamine itself, is responsible for the antidepressant effect. But what is that response? There hasn't been a clear answer to this until now, and it's possible that they simply haven't been looking for it in the right way.
Previous studies that tried to crack the mechanism of action of ketamine, examined the effect of the drug on gene expression in the brain, but not at the individual cell level but at the tissue level. When testing gene expression in a tissue sample that includes cells of different types, possible differences between cells are erased and significant effects may be screened.
Technological developments of recent years allow scientists to measure gene expression in a tissue at the single cell level, thus characterizing differences between cells in the same tissue with unprecedented resolution. In the present study, a research team in the laboratory of Prof. Alon Chen - a joint research laboratory for the Weizmann Institute of Science and the Max Planck Institute - led by the postdoctoral researcher, Dr. Juan Pablo Lopez, used these methods to comprehensively map gene expression in thousands of nerve cells in mice that received a dose of ketamine.
molecular chain reaction
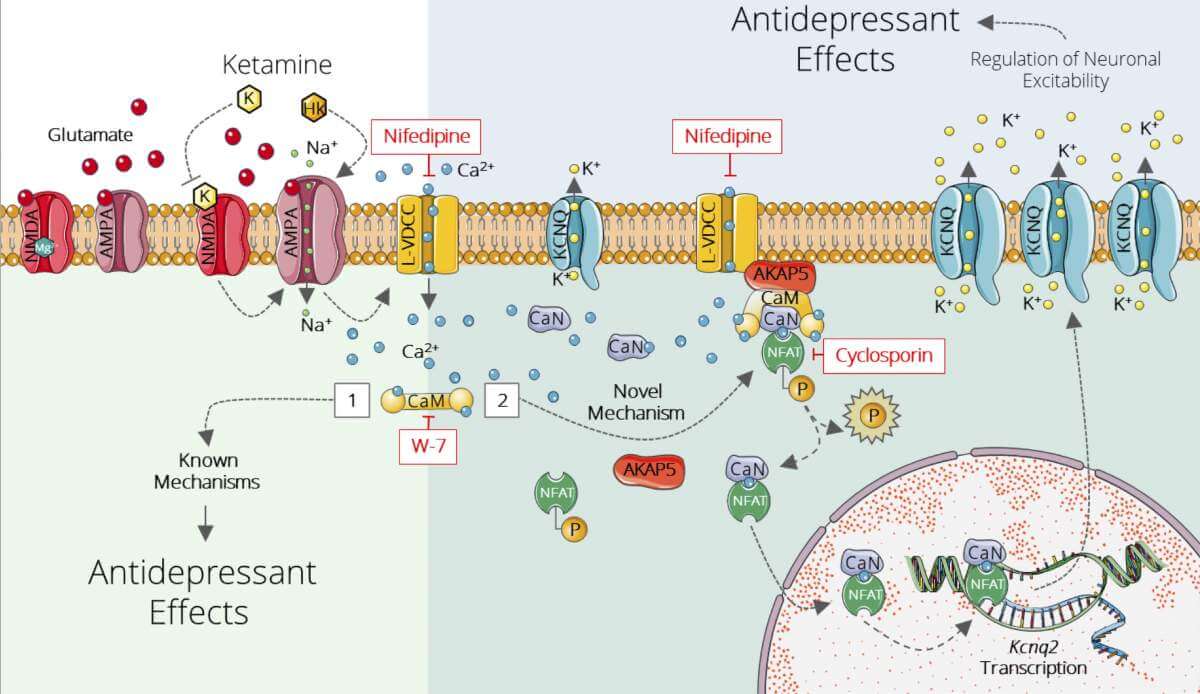
Already in the 90s, it was discovered that unlike the old drugs that act mainly on nerve cells affected by the neurotransmitter serotonin, ketamine affects nerve cells of the glutamate system - another central neurotransmitter. However, given that the antidepressant effect remains long after the drug is cleared from the body, the mechanism of action cannot be attributed solely to ketamine's direct ability to block one of the types of glutamate nerve cell receptors.
"We wanted to understand the molecular chain reaction that occurs following taking ketamine, with the understanding that it is this reaction that generates the long-term effect," explains Dr. Lopez. To this end, the researchers focused on the anterior hippocampus - an area known from previous studies to be an important site when it comes to the antidepressant effects of ketamine.
When the researchers mapped the gene expression of the cells in this tissue in mice, they discovered differences in gene expression between subpopulations of nerve cells that had so far gone unnoticed by scientists. The most significant genetic signature discovered in them was in a subpopulation of cells that showed increased expression of Kcnq2; This gene encodes potassium channels, that is, channels on the cell membrane that open as a result of a change in electrical voltage and allow the passage of potassium ions. These channels play a central role in nerve cells, and are known to be involved in maintaining nerve balance and curbing cell hyperactivity. Through a series of experiments in mice - at the molecular and cellular level and through behavioral, pharmacological, functional and electrophysiological tests - the scientists showed that this genetic imprint is indeed involved in the antidepressant effect of ketamine.
Following the findings, the scientists tried to check what would happen to the effect of ketamine if they added another drug, retigabine, which is known to activate potassium channels in the brain and is currently given to epilepsy patients. The researchers found that the combination of the drugs significantly strengthens the antidepressant effect of ketamine. "A single dose of retigabine was sufficient to enhance and prolong the antidepressant effects of ketamine in mice," says Dr. Lopez. "Furthermore, the combination of the drugs led to a similar effect even in lower doses of ketamine and may make it possible to reduce unwanted side effects." Since both drugs have already been approved by the FDA, the way is paved for testing the effect of their combination on humans in clinical trials.
Hundreds of millions of people worldwide suffer from depression, and hundreds of thousands commit suicide every year. Even after decades of research, this life-threatening disorder is not well understood. "Deepening the understanding of the mechanisms by which antidepressants work is one of the ways to better understand depression - as well as to improve existing treatments," explains Prof. Chen, whose research team led by him revealed a new mechanism of action of ketamine - the most promising drug in the field of depression treatment today. However, despite the great promise, the use of ketamine is limited due to the lack of sufficient data. It is possible that the new findings will help to expand the use of ketamine-based treatments - either alone or in combination with other drugs - and thus more fully realize the new hope for those with depression.
