The blood collected from the umbilical cord after birth has been used for years as a source of hematopoietic stem cells for transplantation. Studies are investigating the possibility of using it to cure diabetes, metabolic diseases, neurological diseases and inflammatory or autoimmune immune reactions
By: Keren Sirota
Umbilical cord blood is the blood remaining in the placenta, and in the umbilical cord adjacent to it, after birth. Until about twenty years ago, this blood was not used at all, and even today, umbilical blood Preserved only in some births. But this small amount of blood has unique properties, thanks to which it is already used today for a variety of medical uses, and is a promise for even more uses in the near and distant future.
Umbilical cord blood contains a large amount of multipotent stem cells. Unlike totipotent stem cells, which can differentiate into all cell types and form an entire embryo, or pluripotent stem cells, which can form all types of body tissues except extra-embryonic tissues (such as the placenta), multipotent stem cells can differentiate into a wide or limited range of cell types. One group of these cells is the mesenchymal stem cells, which differentiate mainly into fat, cartilage and bone cells. Another group is the hematopoietic stem cells, which differentiate into the components of the immune system and blood.
Stem cells derived from umbilical cord blood are currently used to treat about 80 different diseases, and a variety of other uses are in various stages of research. The main use of umbilical blood In medicine today it is a source of hematopoietic stem cells. Transplantation of hematopoietic stem cells is an old accepted procedure for the treatment of diseases in which the blood system has been damaged, such as thalassemia and aplastic anemia, as well as for the purpose of restoring the blood system of cancer patients who have been treated with radiation or chemotherapy (see the article by Jodi and Aryeh Melamed-Katz "Medical Uses" in this issue) . One possible source of hematopoietic stem cells for transplantation is bone marrow from a donor (self or another person), hence the name "bone marrow transplantation". Today, peripheral blood (the blood found in the arteries and veins) from a donor, which has been enriched with stem cells with the help of tumor factors, is used for this purpose. Umbilical cord blood is another possible source of hematopoietic stem cells for transplantation.
Following the progress in the field, public umbilical cord blood banks began operating in the mid-90s. The public banks are established by medical centers, and save the donated blood units for the benefit of any patient who needs them. Private banks also operate, allowing families to keep the blood for the use of the baby and his family only, for a fee. There are currently three public cord blood banks operating in Israel, operated by Magen David Adom, Tel Hashomer Hospital and the organization "Badmich Chai". In addition, several private banks operate in Israel, some of them international. The Ministry of Health recently approved an annual budget of approximately three million shekels for the collection and preservation of cord blood within the framework of public banks, in accordance with the Cord Blood Law, 2007-XNUMX, which was passed in the Knesset three years ago. The implementation of the law should increase the public pool by about a thousand portions every year, as well as create a system of supervision and control over the activities of private banks.
Umbilical cord blood as a source of hematopoietic stem cells
The first evidence that umbilical cord blood contains hematopoietic progenitor cells was published in 1974, and the first transplantation of stem cells from umbilical cord blood was performed in 1988, in a child with Panconi anemia. Since then, the field has gained momentum, and so far over 20,000 cord blood stem cell transplants have been performed.
Cord blood hematopoietic stem cell donation has several distinct advantages over bone marrow donation. When stem cells from umbilical cord origin are transplanted, the risk of rejection is smaller compared to stem cells from bone marrow. One reason for this is the high concentration of regulatory T cells in the umbilical cord blood. These cells, the rarest in the peripheral blood, can prevent inflammatory conditions or heal and control the immune response.
Another reason for the low risk of rejection is the relatively small amount of MHC II molecules in the cord blood stem cells. These molecules play an important role in the inflammatory response, since their function is to present on the surface of the membrane parts of the inflammatory factor (the antigen) against which the system works, thus stimulating the immune response. In a bone marrow transplant, this reaction can lead to graft versus host disease - a condition in which the transplanted immune system attacks the body in which it was transplanted. Cord blood stem cells are also characterized by low levels of costimulatory molecules, such as CD80 and CD86, which also play an important role in increasing the immune response. These characteristics prevent a proper reaction of the various cells, and reduce the immune system's reaction in the umbilical cord blood. Due to the small amount of MHC II molecules and co-stimulatory molecules in the stem cells in the umbilical cord blood, the inflammatory reaction they generate is weaker, and accordingly - the rejection reaction of the graft. In addition, it was found that the secretion of the substances responsible for the graft-versus-host reaction, such as interleukin 2 (IL-2), is smaller in T cells from umbilical cord blood than in a portion of peripheral blood enriched with donor stem cells, and the amount of receptors for these substances on the surface of the hematopoietic stem cells is also smaller in the umbilical cord blood.
The studies indicate, therefore, much lower chances of rejection following umbilical cord blood transplantation, better recovery of the immune system and a reduced risk of graft-versus-host disease. It seems that these benefits are due to the immaturity of the immune system in the umbilical cord blood. The human immune system continues to develop throughout its first years, and at the same time it is exposed to a variety of foreign antigens from the environment; The cord blood, which is of fetal origin, represents an immature and naïve immune system (not yet exposed to foreign antigens).
These properties of the umbilical cord blood mean that a umbilical cord blood transplant can be performed even in a patient whose tissue matching markers (HLA) are not completely identical to those of the donor, without affecting the success rate of the process. The ability to perform a transplant even when the tissues are only partially matched is of enormous importance, in light of the fact that only 40 percent of patients for whom a family member is not found, a suitable donor is found in the donor databases.
Another advantage of cord blood donation is the availability of the dose. The search in the bone marrow donor databases may take between two months and six months, and even when a donor is found, the donation procedure itself is relatively complicated and involves hospitalization and anesthesia. Donating stem cells from venous blood is less invasive, but the main procedure accepted today takes several days, during which a growth factor can be given to the donor to increase the number of stem cells in the peripheral blood - see the article by Judy and Aryeh Melamed-Katz "Medical Uses" in this issue. The umbilical cord blood units are kept frozen in public and private blood banks, and can be available for use within a few days.
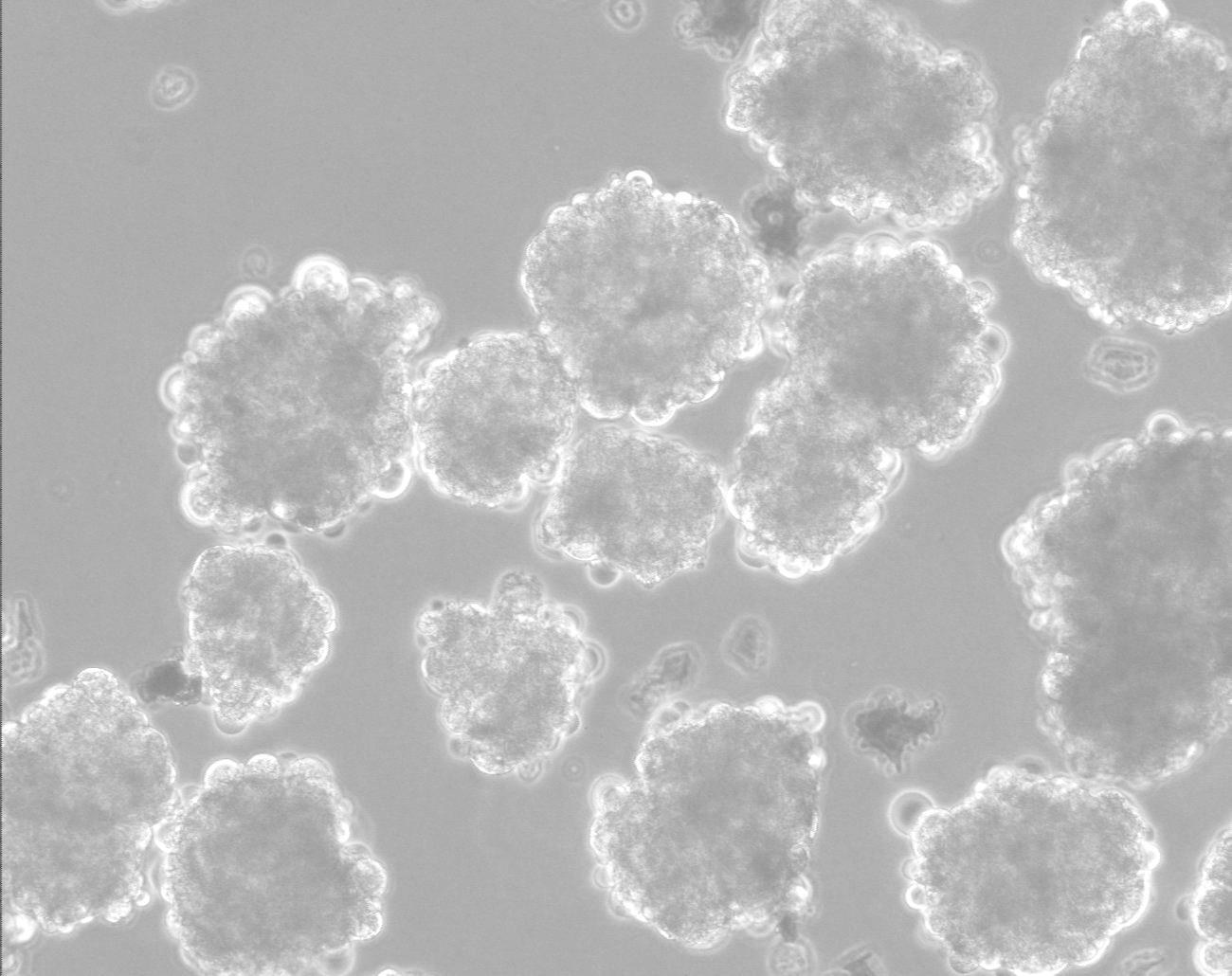
The main disadvantage of the umbilical cord blood used for this purpose is that the small amount of cells in one dose is only sufficient for a person weighing up to about 45 kg (that is, mainly for children). However, studies have shown that a combination of two different blood units, each of which has a partial genetic match to the recipient of the donation, is often absorbed more successfully than one unit, and it was also found that the risk of graft-versus-host disease is less when such a combination is used. Another option is to multiply the stem cells in vitro after collecting them from the donor, and procedures with this goal are currently in clinical trials.
Research and future uses
Apart from the hematopoietic stem cells, there are three other types of stem cells in the umbilical cord blood: endothelial progenitor cells - involved in the creation of new blood vessels and the repair of blood vessels; These cells are in the blood circulation on an ongoing basis, therefore their quantity is relatively high and they are available for transplantation; Mesenchymal stem cells (mesenchymal stem cells) - these cells are the most suitable for use in tissue engineering, because they can differentiate into several types of cells, including cartilage, bone, fat and connective tissues; and embryonic stem cells. The fact that fetal stem cells are also found in the umbilical cord blood was only discovered a few years ago, due to their small number and small size, and only recently was a protocol formulated for their isolation. These cells can actually form any type of tissue.
In general, the "young" nature of the stem cells from umbilical cord blood compared to stem cells derived from the bone marrow or peripheral blood of an adult make them much more convenient for research purposes. their long and stable telomeres (telomeres are the DNA regions found at the ends of chromosomes, which break down and shorten during the life of the cell and thus are involved in determining its age and lifespan); Their increased tendency to divide and reproduce, and their genetic stability over time, that is, their lesser tendency to accumulate oncogenic (cancerous) mutations compared to stem cells from bone marrow - all these make them an ideal tool for research in general and research in tissue engineering in particular.
One of the directions in the field of tissue engineering is the use of stem cells in the treatment of juvenile diabetes, a disease caused by autoimmune destruction of the pancreatic cells responsible for insulin production. The stem cell treatment is designed to encourage the production of new pancreatic cells, and to prevent the autoimmune destruction of the existing cells. So far, it has been shown that autologous transplantation of hematopoietic stem cells, combined with intensive suppression of the immune system, resulted in the complete recovery of most patients from the disease (that is, to insulin independence). The rationale behind such a combination of immunosuppressive treatment and autologous transplantation of hematopoietic stem cells is to bring about a kind of immunological reset, thus inhibiting the autoimmune activity. Experiments of this kind with stem cells from umbilical cord blood are just at the beginning and are mainly done in children.
Interesting developments in the study of the uses of stem cells from umbilical cord blood were also recorded in the treatment of neurological diseases such as stroke and spinal cord injury. In experiments conducted in the transplantation of stem cells in the damaged areas, the researchers hoped that the transplanted stem cells would differentiate, become nerve cells and integrate into the damaged tissue. However, the findings show that treatment with stem cells from umbilical cord blood has diverse beneficial effects even when there is no evidence that the cells themselves have integrated into the tissue. Most experiments of this type were done in animal models (animals), and the findings indicate that the transplantation of stem cells from umbilical cords has beneficial effects without side effects: a certain neuroprotective effect (that is, a reduction in the extent of damage to the existing tissue - preventing the death of existing neurons, neuronal rescue), and a functional benefit in relevant behavioral tests. These effects were also accompanied by a decrease in the inflammatory response and a reduction in the extent of ischemic damage (i.e. the damage to the blood supply) in models of stroke and other neurovascular diseases. Recently, a transplant of stem cells from umbilical cord blood was reported in a patient with a spinal cord injury. The treatment resulted in an improvement in nerve, sensory and motor activity, and tomography (CT) and magnetic resonance (MRI) scans indicated regeneration of the spinal cord in the affected area.
A completely different research direction focuses on the immunosuppressive properties of umbilical cord blood. As already mentioned, one of the prominent advantages of umbilical cord blood is the high concentration of regulatory T cells, which can prevent or cure inflammatory conditions and control the immune response. Until recently, the use of regulatory T cells was very problematic due to their low concentration in the peripheral blood, what is more, with the existing methods they cannot be isolated without harming their animals. Umbilical cord blood, where these cells are found in much higher concentrations, allows for the first time to examine the medical possibilities inherent in the use of these cells in the treatment of a variety of diseases, including hematological, neurological, endocrine, heart diseases, hereditary diseases and autoimmune diseases.
Several animal and human experiments tested the anti-inflammatory effects of umbilical cord blood in the animal body. One example is an experimental treatment for a cardiac complication called chronic right ventricular volume overload. Injection of stem cells from umbilical cord blood improved heart function, increased the formation of new coronary blood vessels and reduced the local inflammatory response. Another experiment suggests that even lung damage due to hyperoxia (hyperoxia-induced lung injury) can be treated in a similar way. Additional experiments are conducted in "humanized mice" - mice that have been engineered so that their immune system more closely resembles that of humans. All in all, it seems that treatment using stem cells from umbilical cord blood can control and moderate an inflammatory or autoimmune immune response, when the mechanism is complex and involves, among other things, a decrease in the levels of the cytokine interleukin 2 (2IL).
In addition to this, it should be noted that the transplantation of hematopoietic cells can also be suitable for the treatment of diseases that are not related to the blood system, such as hereditary metabolic diseases in which a defect in a certain joint enzyme causes the accumulation of toxic substances in the tissues. The currently accepted treatment for most of these diseases is the use of an enzyme produced in a laboratory for this purpose and injected into the patient. The main disadvantage of the method is that the injected enzyme cannot cross the blood-brain barrier, which is actually the dense structure of the endothelial cells that make up the blood capillaries in the brain. This barrier (as well as barriers between other organs in the body) can only be passed by molecules that are soluble in fat or that have a specific receptor, so enzyme injection is not a suitable treatment when the enzyme deficiency is also cerebral. In such situations, the only treatment that has achieved results to date is the transplantation of hematopoietic stem cells, including monocytes, which are able to cross the blood-brain barrier and produce the missing enzyme there.
It is important to emphasize that the uses described in this section are still in an experimental framework, and many more clinical studies will be required, especially those that include long-term follow-up of patients, before they join the arsenal of accepted treatments offered to the public. The potential of using umbilical cord blood depends on another question, to which there is no clear answer, and that is - how long the dose is kept. Although theoretically, the cells frozen at a temperature of minus 196 degrees are supposed to keep alive for several decades, in practice, since the first portion of umbilical cord blood was frozen in 1988, experience cannot testify for more than twenty years.
Stem cells from umbilical cord origin have therefore been proven to be effective in the treatment of a large variety of diseases, but their main use today is in the treatment of hematological diseases. Their use for this purpose becomes an acceptable alternative to bone marrow transplantation, thanks to the reduced risk of rejection and other complications, the high chances of success even in the absence of a perfect genetic match, and the high availability of the doses. More and more families around the world choose to keep the baby's umbilical cord blood despite the costs involved, as a kind of "biological insurance" for the baby and his family. However, despite the variety of current and future uses of umbilical cord blood, umbilical cord blood is still collected and preserved in only 5 percent of all births in the world, a fact that indicates that the field is still in its infancy, and there is still a long way to go.
for further reading:
Francese, R. and Fiorina, P., "Immunological and Regenerative Properties of Cord Blood Stem Cells", Clinical Immunology (2010) In press.
Glucknam, E. and Roche, V., “Cord Blood Transplantation: State of the Art”, Haematologica 94:451-454 (2009).
Harris, DT, “Non-Haematological Uses of Cord Blood Stem Cells”, British Journal of Hematology 147:177-184 (2009).
Prasad, VK and Kurtzberg, J., "Cord Blood and Bone Marrow Transplantation in Inherited Metabolic Disease: Scientific Basis, Current Status and Future Directions", British Journal of Hematology 148:356-372 (2010).
< <<Credit>>
Keren Sirota has a master's degree in life sciences from Tel Aviv University. kerensirota@gmail.com

6 תגובות
Umbilical cord blood in a private bank is reserved only for you according to your need. It is public, free of charge, but not guaranteed only to you in case of need. If someone needs a dose, they will bring it to him if there is a match, if from other parts of the world that the banks are in contact with...
In any case, in my opinion, you should press for them to take your portion to one of the banks if you do not do private, because most likely it will be suitable for one of the family members if they need it...
Interesting article, but I still couldn't fully understand what is the advantage of keeping cord blood in a private bank over a public blood bank?
Thanks for the information. The obvious question is why doesn't the state start a campaign encouraging people to save umbilical cord blood at birth? There are quite a few companies in this field, so the cost of the process is also not sky high... Instead of bothering with the important things, they recommend us to take a swine flu vaccine...
It is hard for me to believe that umbilical cord blood is preserved in 5 percent of births in the world, and not even in 5 percent of births in the Western world. This is an expensive and rare procedure and is not accessible to most of the world's population.
In the calculation of cost versus benefit, I don't know how much it is worth.
My question is this
In standard births in hospitals, the newborn is disconnected from the placenta before the placenta "dies", meaning that there are still heartbeats that transfer the blood from the placenta to the newborn, in the case of home births the midwife prefers (for the most part) to let the placenta circulate all the blood to the newborn and after the heartbeats stop Severing the umbilical cord - that is, all the blood from the placenta has passed to the newborn, there is a claim that claims that children who have been separated from the placenta after the last pulse of the placenta come out healthier and more immune to diseases and because of this their natural immune system is strengthened than that of newborns who were severed "prematurely"
Thoughts and ideas will be gladly received
Definitely an interesting article