Mature stem cells in the pancreas were supposed to help deal with diabetes. The problem is, there probably won't be such a match
During the life of most tissues in the body, cell turnover occurs: old cells die and young cells take their place. The question of how the different tissues produce and maintain the necessary amount of cells is one of the basic questions in biology. In recent years, the opinion has been formed that different tissues contain stem cells, which are capable of differentiating into each of the tissue cells and replacing them when they are damaged or dead. Since these stem cells have already undergone initial differentiation into cells suitable for a certain tissue, they are called "mature stem cells"; This is different from the embryonic stem cells, which have not yet differentiated. Scientists have high hopes for adult stem cells; Mainly considering the moral problems in the production of embryonic stem cells; These cells are extracted from embryos in early stages of development.
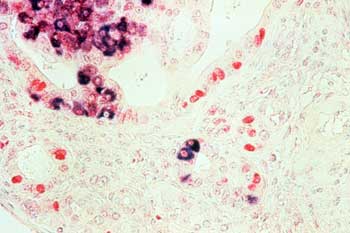
It is now clear that adult stem cells play a central role in the creation and maintenance of blood, skin and intestinal cells. This was the accepted assumption regarding the pancreas as well. In the pancreas there are special cells called beta cells, which are sensors for the blood sugar level and secrete the hormone insulin into the blood as needed. Insulin causes cells in the body to store sugar reserves. In juvenile diabetes patients, the immune system destroys the beta cells and as a result the patients are dependent on daily insulin injections. The need for new beta cells to be implanted in the body of patients is critical - this is the only possibility to cure millions of diabetics in the world. But due to the high prevalence of diabetes there is a very high demand for beta cells and there are not enough cells for transplantation. The cells intended for transplantation come from people who have already died, and they can be used only a few minutes after death.
Theoretically there are several ways to increase the supply of beta cells for transplantation. One way is to encourage the division of the remaining beta cells in the pancreatic tissue, but efforts in this direction have not borne fruit so far. Alternatively, it is possible to use embryonic stem cells, which have unlimited division potential, and direct them to differentiate into beta cells. The research in this direction has not borne any significant fruits so far, what is more, in many of the western countries, and the United States in the first place, severe restrictions are imposed on the work with these cells for ethical reasons.
A third way is to isolate mature stem cells from the pancreas, which are naturally designed to create new beta cells. Working with such cells will avoid the possibility of rejection, as well as the need to use embryos for research. Based on research findings and circumstantial evidence, it was suggested that the pancreas also has mature stem cells. Due to the great medical potential, many researchers in the world are devoting a lot of effort to their identification and isolation, and millions of dollars are invested in establishing centers for researching adult stem cells and testing the possibility of transplanting them into diabetic patients, so far without results.
Recently, a study was published by the Israeli researcher Dr. Yuval Dor in the laboratory of Prof. Douglas Melton from Harvard University, which casts doubt on the existence of mature stem cells in the pancreas. Dor showed that new beta cells in adult mice are generated by division of existing beta cells and not by differentiation of mature stem cells. The study was published on May 6 in the journal "Nature", received an accompanying article and caused widespread resonance in the medical research community.
The research was conducted in mice knowing that the biology of the pancreas tissue in mice and humans is almost the same, and we can therefore learn from the results in mice about the corresponding system in humans. The method used by the researchers is called "genetic lineage tracing", and it is possible to irreversibly mark cells in the mouse's body and follow their fate long after the marking. The researchers marked 30% of the beta cells in the pancreas of young mice, and a year later they checked the frequency of the marked cells in the pancreas.
If new beta cells in the pancreas are generated from stem cells, the expectation was that after a year the frequency of labeling would decrease because they had developed from stem cells that were not labeled at the beginning of the experiment. If new beta cells are created as a result of division of existing beta cells, the proportion of labeled cells in the pancreas is not expected to change. And the result: the frequency of the marked cells remained as it was after one year (a period of time corresponding to thirty human years).
Later, the researchers performed another experiment. After marking the beta cells present in the mouse, two thirds of the pancreas were excised. As a result, an "emergency situation" was created in the pancreas. It was common to think that in such a stressful situation reserves of mature stem cells are mobilized, which contribute significantly to the creation of new beta cells. However, in practice it turned out that even in this emergency situation, the new beta cells created in the pancreas contained the marking, that is, they originated from existing beta cells, which survived the operation and divided into additional beta cells. From these experiments it became clear that within the pancreas new beta cells are created from existing beta cells without any evidence of the contribution of mature stem cells. The researchers emphasize that the study does not rule out the possibility that mature stem cells exist in the pancreas, but their contribution to the creation of new beta cells is marginal.
Prof. Melton, who directed the research, says that the findings will undoubtedly affect the future direction of research to find a treatment for diabetes. "The clinical direction for curing diabetes will now be based on finding a way to enhance the ability of beta cells to divide," he says. According to him, if the patients have beta cells left in the pancreas, this possibility should be based on this possibility, but if the patients do not have beta cells left in the pancreas, the meaning of the findings is that the only source of new beta cells will most likely be the embryonic stem cells."
