Our current technology in the field of biomedicine is basically fifty years old and more. It is not always the right answer to make things smaller, because this often creates problems * We desperately need thinking outside the box for an overall change in the field. *Roey Tsezana continues to report from the life sciences conference in Antwerp and prepares for his lecture today
Tuesday, seven in the morning. The alarm clock screams hysterically, and I open my eyes and feel as if I woke up several hours early. The sun has not yet risen in Belgium, and although the curtains are drawn to the sides not even a sliver of light penetrates into the room. I drag myself to the shower, get dressed and go down to the hotel dining room. Cornflakes with milk, a small bun with cheese and an omelette, and I'm ready for another day of lectures.
Already in the first seminar of the morning you are faced with a difficult choice between rehabilitation medicine and biomaterials. In the end, I decide that I was sent to the conference for a specific reason - to hear about advances in my research field and to make external contacts - and give up the seminar in rehabilitation medicine, which actually seems very interesting in general. The lectures in that seminar cover a wide range of topics: human-machine interfaces through electrical reading of the brain, improving speech understanding in people who have had hearing aids implanted in the bones of the ear, developing biological prostheses for amputees and improving walking with a robot. So I gave all that up, and went to the Biomaterials I seminar, with a slight sense of sacrifice.
I arrived just in time for the start of the first lecture. Fortunately the speaker, whose name I shall not mention, started slowly. He told about all the different types of universities in Hanover, Germany. Oh well. But he continues - what is this institution, what is this institute, and where did this university come from. And only after a few minutes in which he was able to completely destroy any trace of vigilance that still existed in the audience by mistake, he arrives at his research. It's only half past eight in the morning and he's talking monotonously and with a strong German accent about poly-capro-lactone (PCL) panels and how to sinter them. What interests the audience about as much as it probably interests you, dear readers. Why sinter them? Do not know. What is sintering? Well, I actually know that, but he didn't even bother to explain. But at least I now understand the hierarchical structure of the research institutes in Germany, and why his university is the most successful.
The second speaker - Mr. Havigen - was already more fluent and described how he is trying to create biomaterials for bone implantation, which can survive and not collapse under the considerable force exerted on the bone. Those biomaterials will house mesenchymal stem cells that will restore the bone, and it seems that he already has partial success in this direction, with a scaffold composed of a combination of titanium and nickel. Nickel-titanium scaffolds, it turns out, are able to withstand the compressive and tensile forces applied around the bone, and even support the stem cells inside them. In his latest slides, Avigen showed that mesenchymal stem cells seeded on the scaffold respond to stress and secrete a large amount of interleukins.
At least, he thought he showed it until the questions started coming from the audience. "Are you sure that your method of measuring force really takes into account the flow inside the scaffold?" "How do you know your measurements are fine enough?" There were the more subtle questions, which were enough to make the poor PhD student squirm like stage-wounded diarrhea and hide like a threatened turtle behind the podium. I can't blame him. The questions were really spot on, but it is not easy to formulate a simple and clear answer in a language that is not your mother tongue, especially when you are facing a horde of angry professors who know much better than you the research topic, the research methods and where anything and everything can go wrong.
The next speaker is Mr. Rothwell from the University of Dundee in Scotland (but without the fun accent), who came to tell us about a stent for intestinal leaks. A stent is a type of small tube designed to support the walls of blood vessels or intestinal tubes from the inside. Leakage in the intestine, it turns out, can occur as a result of a tear in the intestinal wall or surgery on the intestine, and is one of the most serious complications that can occur after a tear or surgery. Such a leak can result in a mortality rate of almost 40%. Rothwell's idea is to create a stent that can be placed inside the intestine to hold the walls in place and allow them to heal. Some of the immediate advantages of such a stent include the fact that the patients will be able to be fed immediately after the placement of the stent in the intestine, and of course - it will greatly reduce the incidence of leaks. The stent itself will be made of a material that breaks down by itself in the body after some time, so that it will not be necessary to re-enter the intestine to remove the stent.
After Rothwell, Mrs. Valerinho from Portugal comes up and tries to explain about her new invention - the implantation of a substrate made of nanofibers in the wound area, which will help complete recovery. It turns out that in the event of an injury to the body, fibroblasts penetrate the resulting space and quickly fill it with scar tissue that prevents true and complete recovery. Added to this are cells from the immune system that cause an acute inflammatory reaction in the area - which is not always a good thing.
Valerinho used a method called electrospinning to create nanofibers - and at this point I began to give her my full attention, because this is the method I also work with, and tomorrow I will have to explain myself on a similar topic. In any case, Valerianho created a substrate of nanofibers made of a polymer called polyethylene terephthalate and implanted it into wound areas in mice. The substrate did not allow the cells of the immune system and the fibroblasts to penetrate through it into the area of injury, thus preventing the formation of scar tissue. On the other hand, it also did not allow the blood vessels to grow into the area - which calls into question the usefulness of the entire invention, especially when you take into account the fact that a substrate made of such a polymer takes a very long time to degrade.
Perhaps this is the time to tell that after each short lecture at the seminar, Mr. Wilson's hand (the one who lectured yesterday about academia and industry) raised his hand to ask a particularly difficult question. I really hope he doesn't show up at my seminar tomorrow, or at least eats a good lunch before the seminar.
And if we're already talking about scary stories, the student from the Technion has already shared with me a horror story from a seminar that happened yesterday on the topic of computerized image processing. One of the lecturers at the seminar presented a particularly problematic work, which hardly used statistics, or serious tests to measure pain in the patients. When she finished the lecture, the hands of most of the audience went up, and the poor thing almost fainted. Perhaps it would have been better for her to pass out, because instead she went into a panic on stage and was unable to answer any questions.
Oh my god, and I don't even have a tie yet…
But still, I've been through more than enough lectures in the past and I know how to prepare! The break after the seminar is used to check the room where I will speak tomorrow. There is a podium behind which the lecturer stands, a large screen and dim lighting. I talk in advance with the person in charge of the room and make sure that the lecture conditions can be adjusted for me. I have some unusual requests, I admit, but this is my lecture and I need to feel comfortable. One of the things that particularly bothers me is that all the lecturers stand behind the podium. which is adapted to Americans and Europeans who are ten centimeters taller than me on average. I prepare the microphone in advance so that I can stand to the side of the podium and not behind it and make full use of body language. Adjust the lighting a little better so that there is more light on me (but not too much, so that it doesn't dazzle) and make sure that the presentation works on the computer, that I can connect the wireless remote and that it does work from all corners of the room.
I know it sounds like I'm panicking and to some extent I really am, and that's a good thing. My weaker performances are precisely when I am not stressed enough for the performance and do not prepare for it from all angles. The great Mark Twain said at the time that, "There are only two types of lecturers: those who get excited before the lecture and those who lie". Although I have already given more than enough lectures in front of much larger audiences, I still get excited before each new event. I harness the excitement and pressure to my advantage, try to pay attention in advance to every detail that can enhance or degrade the performance, and always remember that when I'm on stage, I'll be fine.
Brain machine interfaces
From here we continue to Phil Troik's Honorary Lecture on Neural Prostheses. I already recorded Troik's previous lecture on the electrodes that connect to the brain, but in the current lecture he gave a much broader overview of the field of neural interfaces. It turns out that there is a long list of diseases and injuries that are being tried to be treated using neural prostheses, whether in a brain-machine interface, neuromodulation or other interfaces.
Ancient prostheses already existed in ancient Egypt, but since then we have made some progress. Especially recently, prostheses are everywhere in medicine. They restore hearing in deaf people through ear implants - electrodes placed in the cochlea and restore the ability to hear to many people. Robotic limb prostheses are also very easy to manufacture today - much easier than understanding how to control them.
Brain-machine interfaces have gained popularity and are used to move wheelchairs or shapes on the screen. According to Troik, this is a big paradigm shift, because even a decade ago there was a big debate about whether we should even integrate electronics into the brain. Today there is a fairly large consensus that we can put into our brain and body whatever we want - as long as we are able to perform the required function.
Already today there is a wide variety of technologies designed to provide images to the brain. Science and science fiction go hand in hand here, and the public has a lot of misunderstanding about what can really be done. And according to Troik, "I'm pretty sure I could go out on the street and convince almost anyone that we are capable of doing almost anything about the human body and brain." And the truth is that he convinced me of it without even trying.
Troik quickly reviewed the new prostheses and those of the last fifty years, then posed the million dollar question: Are there problems common to all these prostheses, and do they really deserve our attention? And the answer is that it definitely is: there are common problems and they are all about the interface.
There are four different types of interfaces. The first is the electrode-nerve interface, and according to Troika, it is enough to work only on this interface in the next decade to achieve important progress. The main problems in this interface are divided into the reception of the neural message and the transmission of our own neural message. To achieve optimal reception, we need to place the tiny electrode in exactly the right place in the brain. This problem is also shared by the issue of the optimal transmission, which should take place in the right place and at the right time.
The basic idea of an electrode-nerve interface is simply a piece of wire stuck in the tissue, with a current running through it and activating the neural material around it. But there is a problem here: the electrode works on an electric current - electrons - while the nerves work on an ionic current. How does the electrical electrode inject charge into the neurons? The answer is the electrode is used as a transducer that converts an electronic current into an ionic current. To do this there is a need for faradaic reactions (which is a concept that requires a lecture in itself) occurring around the electrode, and these reactions must be reversible to protect both the electrode and the tissue. This is where the real challenge in designing the electrodes begins, among other things because of the safety effect. An almost inevitable by-product of the Faradian reaction is the decomposition of the water in the tissue and the formation of gas. You don't have to have a developed imagination to realize that water turning into a large volume of gas at high speed will not be good for the neurons inside of which this happens (in other words, the neurons will simply explode from the inside).
In the AIROF electrodes, the Faradian reactions are limited to a thin layer in the electrode made of iridium and platinum, from which the ions are formed. The problem is that when the electrodes produce a certain voltage of 3-5 volts. It is not clear who is absorbing this tension. And according to Troik, "The electrochemists don't want it because it will damage their electrodes. The biologists don't want it because it will damage the tissue and cells. The neurophysiologists are not ready to accept it because it will damage their delicate neurons. So where does this tension go?"
What else remains to be improved in the electrode-nerve interface? "I believe that we need to adapt the surface of the electrodes so that they attract the neurons to them - something that will surely be simpler than designing mini-robots that will travel through the brain and attract the electrodes to the right neurons. We need to improve the ability to inject the charge by an order of magnitude, and if we are not careful the electrodes could destroy the tissue around them. We need to consider new structures that will focus on new nanofluids that can activate the neurons without electrical activation."
The second interface according to Troika is electronics-biology. As an example of this interface, tissues can be coated with electronics, but since a water/ion environment is destructive to electrodes, this does not seem likely at the moment.
And speaking of the relationship between water and electrodes, at this point Troik expanded on another area that is not fully understood by most of the public. To protect the body of the electrode, a polymer is often used. The problem is that the polymer does not completely block the water. Water diffuses rapidly through any polymer we have, so polymers are unable to act as an effective boundary. Today, the lifespan of a polymer sheath can be predicted by its size and its permeability to ions. We can make a pacemaker that has a life span of thirty years, but as the devices get smaller, their life spans get shorter. Therefore, it is naive to think that only wrapping in polymers will advance the field to a serious extent.
"The hermetic signature of an electrode is nothing more than an illusion," Troik said, adding that, "new coatings must be defined that will abandon the idea of a hermetic signature. We need to stop reinventing the wheel - groups need to cooperate with each other and not invent things that have already been done in the past."
The third interface is a transdermal interface. A coil outside the body creates a magnetic field, and the implant inside the skull picks up the changes in the field and reacts accordingly. There is at least one group trying to advance this field, and Troika is involved in their research. It is difficult to deal with the efficiency of the coil and the external field, for the simple reason that a lot of energy is needed to continuously activate electrodes inside the brain. According to Troik, even if we had batteries powerful enough to power internal electrodes in the brain, the field of neurophysiology would probably not benefit from it, but we would use it to solve the world's energy problems.
The problems that still exist in the third interface are that the small size of the electrodes causes poor magnetic coupling. It is also not clear how it will be possible to achieve a two-sided broadcast. The electrodes cannot easily transmit information back. A 10-fold improvement in energy utilization and working with different wavelengths is needed to reach the desired capacity. Beyond that, it is also not clear what the magnetic field will do to the biological tissue!
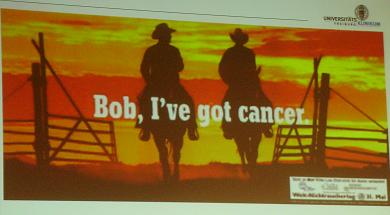
In conclusion, most of our current technology is basically fifty years old or more. It's not clear that the right answer is to make things smaller, because that often creates problems when using current manufacturing paradigms. Current efforts are focused on streamlining 20th century technologies, and we desperately need out-of-the-box thinking for an overall change in the field.
The fourth, final interface (and the one that really made everyone stop and think for a moment) is the user-engineer interface. This interface raises the really important questions that many biomedical engineers seem to be trying to avoid today. What is the threshold of use for neural prosthesis? At what stage do you need it, and when can you be satisfied with a living stick? What are the real needs of the users? Troik strongly argues that engineers should be less technology-oriented and more biology-oriented. As a good example, he cites a lecture he recently heard from a professor in California who is confined to a wheelchair and almost completely disabled.
When Troik explained to the professor about a new prosthesis that helps with bladder control, the professor asked, "What does a bladder prosthesis do for me? I have a catheter attached at all times, with a storage bag. If you gave me a prosthetic bladder, I would have to go to the bathroom - and then you would have to design prosthetic hands for me as well."
In my honest opinion, Troik hit a very correct and very painful point here. Many of today's biomedical inventions require a huge investment of resources and suffering on the part of the patient, and although the results may improve his objective state of health, sometimes they also complicate his life. As another example of this, another invention that won the 2008 Biomedical Congress Award: a robot designed for people suffering from severe tremors, constitutes an exoskeleton for the hand and is capable of vibrating at a frequency opposite to the body's own vibrations. The result is an 80% decrease in the intensity of the vibrations and the opening of the door back to normal life for some of those people - who are unable to even lift a glass of water to their mouth.
Well, it turns out that very few people are willing to use a robot for the simple reason that it is too massive, too threatening, and they are afraid to walk around the street with it and be seen as a RoboCop prototype. It's a bit hard for me to understand, because it's always been my dream, but the point is that the engineers should think less about the technological capabilities and more about how they can be integrated into the existing company.
The truth is that there is much more to tell, but my lecture takes place tomorrow at noon, and it is already late at night. You have to prepare to succeed. Tomorrow you can read how the lecture was, see revealing photos of me in front of a crowd of bloodthirsty engineers and read what the patent is all about.
Don't miss the grand finale of... "PhD student on the road!"

2 תגובות
Roy, it's great fun to read and be a partner in your professional and personal experiences. Good luck in the lecture tomorrow. We're crossing fingers for you
Good luck Roy.