On a natural barrier that interferes with the reprogramming of pancreatic cells
With hundreds of millions of patients around the world and no cure possible, it is no wonder that diabetes is the focus of attention of many research laboratories. One of the promising directions for future treatment of diabetes is the reprogramming of cells in the pancreas so that they replace the insulin-producing cells whose activity has gone awry. Reprogramming of cells is already done today under laboratory conditions, but with only partial success. Weizmann Institute of Science scientists revealed recently a natural barrier that interferes with the reprogramming of pancreatic cells; This discovery may pave the way for future treatment of diabetes.
Diabetes has two main manifestations: type 1 diabetes ("juvenile diabetes"), which is usually diagnosed at a young age and results from an attack by the immune system on the insulin producers in the pancreas (beta cells), and type 2 diabetes, in which the beta cells gradually collapse under the load - Excess demand for insulin. There are currently various treatments, including insulin injections, against the symptoms of the disease, but in many cases the diabetes continues to worsen, and may cause serious complications. In recent years, as part of an experimental treatment, donated beta cells are transplanted into type 1 diabetes patients, but this treatment is not optimal: both due to the existing shortage of cells for transplantation, and in light of the fact that, as with any organ transplant, the patient must take drugs that suppress the immune system in order to prevent rejection of the transplant .
Another research direction that inspires new hope is, as mentioned, the reprogramming of cells in the pancreas. In recent years, scientists have discovered that mature cells in our body are not as "fixed" in their final form as previously thought. Many research groups around the world are currently engaged in returning adult cells to the state of stem cells, while other research groups, including the research group of Prof. Michael Walker From the department of biomolecular sciences at the institute, they focus on the possibility of reprogramming cells for different purposes. Recently, Prof. Walker's group tried to reprogram the "production lines" of the pancreatic cells that produce digestive enzymes so that they replace the beta cells in the pancreas whose activity is affected by diabetes; These cells are good candidates for reprogramming, since both their location and the origin of their development are similar to those of beta cells, and apparently "turning on" or "turning off" a handful of genes is enough to effect the change of purpose.
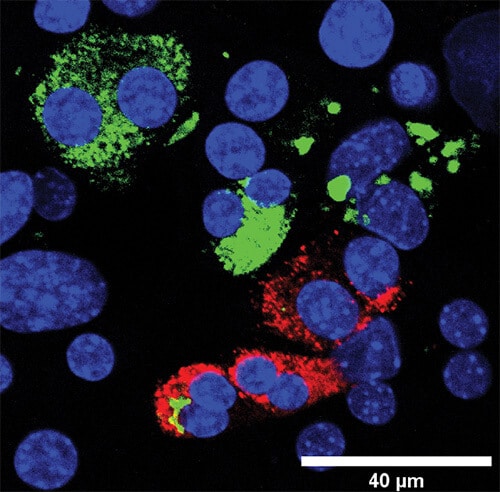
The researchers, led by post-doctoral researcher Dr. Ofer Elhanani, grew pancreatic cells in the laboratory and inserted into them transcription factors - molecules that turn on or off groups of genes - related to the insulin production capabilities of beta cells. To identify which cells had begun to change and become beta cells, they added a fluorescent tag that glowed only in the cells that produced insulin.
When some of the cells glowed, the researchers separated them from the rest of the cells using flow cytometry, thus creating two groups of cells: those that "turned their skin" and were reprogrammed, and those that remained their own. A comparison between the two groups revealed that the difference between the cells lies in the presence of another transcription factor known as REST. This transcription factor is expressed in pancreatic cells that secrete digestive enzymes - but not in beta cells. When the scientists blocked the activity of this transcription factor, the reprogramming process was much more efficient.
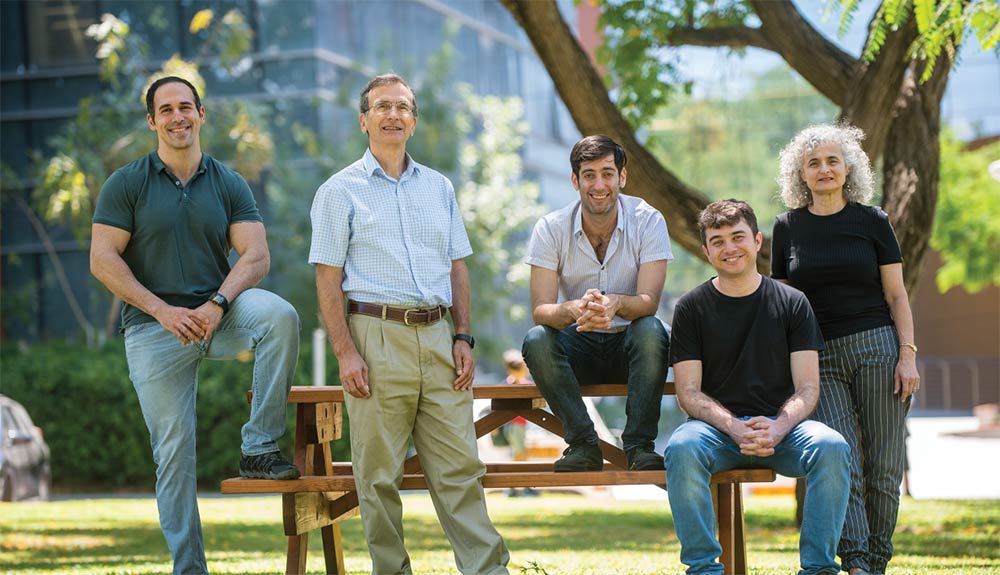
From the right: Dr. Dina Leshkowitz, Itay Vaknin, Dr. Ofer Elkhanani, Prof. Michael Walker and Dr. Tomer Meir Selma. Barriers are removed
Later, the researchers discovered how REST prevents key genes in beta cells from being expressed in the other pancreatic cells: it binds to certain essential genes near the binding sites of the transcription factors that the scientists used, thus blocking their activity and silencing the genes. "In order to effectively reprogram cells, the process must first be understood in its molecular details and the natural barriers that prevent it from occurring in normal cells," says Prof. Walker. "Identifying REST as such a barrier provides us with new tools to create cells that produce insulin." Adds Dr. Alhanani: "Although many obstacles are expected in the transfer of this basic knowledge to the medical service, discovering the reason why something does not work as expected is the first step on the way to correcting it."
Also participating in this study were Dr. Yonatan Sobel, Lital Pobodovsky and Iti Vakanin from the Department of Biomolecular Sciences, Dr. Tomer Meir Selma and Dr. Dina Leshkowitz from the Department of Life Science Research Infrastructures - and Dr. Dror Kolodkin-Gal from the Hadassah University Medical Center.
Science books
98% of the secretory cells in the pancreas produce digestive enzymes, only 2% produce insulin.

2 תגובות
And how long will it take to treat the poor?
Probably another decade
In any case, go up and succeed...we are waiting for you.
When will you start treating the real cause of diabetes?