Printing replacement organs in a way that will allow them to be implanted in a person's body and to be integrated into his operation

At the age of ten, Luke was faced with two options that children are not usually forced to choose between: a kidney transplant, or a short life with frequent visits to the hospital to treat his failing kidneys. His parents chose the third option: an unusual and experimental surgery. Prof. Anthony Atla of Wake Forest University collected cells from Luke's bladder and grew them in the laboratory with patience and love. Together with his research team he created a scaffold for them: a ball of synthetic polymer in the shape of a new blister. The researchers lined the synthetic bladder with muscle cells on the outside and cells that cover the natural bladder on the inside. They watched the natural-artificial organ for weeks while it was in a bioreactor in the laboratory, and knew that the cells were multiplying and breathing real life into it. Finally they implanted it in young Luke's body[1].
The boy regained his life.
Today, Luke still enjoys good health. The revolutionary treatment at the time - the creation of an entire replacement organ - was fully successful[2].
What if we could do this to other organs in the body?
The answer - at least, one possible answer - was provided to me by a respected professor of medicine a decade ago. The same professor prophesied to me that the day is not far when we will be able to replace the organs of the body, organ by organ.
"Has the heart gone bad?" He said, "We will replace him. Did the kidneys break down? them too. Are you not satisfied with the condition of your skin? It will also be possible to treat him."
The result of this situation would be, in his opinion, the stopping of aging in all practical respects. We can argue about the small details in the vision, but it is clear that when we can replace every tissue in the body, many of the diseases that bother us today will appear to us in the future as trifles that can be treated. Unpleasant trifles, perhaps, but just as we go to the dentist today and are willing to suffer for the sake of health, so in the future we will also be willing to go to the 'tissue engineer' at the hospital to extend the duration of our healthy lives in a decade or two.
Well, a vision is a good thing, but you don't pay with it at the grocery store. The question arises, therefore, to what extent we can currently find alternatives to tissues and organs, what are the major challenges in the field - and when will we really reach the promised land of endless health.
Let's start with the least impressive alternatives at first glance: the inanimate replacement organs.
Rickard Normack was close to middle age when he lost his arm in a work accident. He received a prosthesis - a traditional prosthetic arm. That arm, which was his ticket to the world of replacement organs, was attached to the stump area with a sleeve that was supposed to be customized for him.
That, at least, is the promise. The reality is less pleasant: it is difficult to find a convenient way to connect the prosthetic organs to the body, and Normak could not get used to the new prosthesis[3]. He did not activate it well. She was, quite simply, a dead limb.
In this respect, Normak's story is similar to the experiences of many who are forced to replace their biological-original arms with a plastic-metal organ. Most arm prostheses today are simple in nature. The simplest ones resemble an elongated hook that can be closed by moving the elbow or shoulder in a way that causes the ligaments in the prosthesis to stretch. The more sophisticated ones are able to receive electrical signals that usually come from the nerves in the chest area, and translate these nerve signals to drive the artificial joints and 'muscles'. These also suffer from the same problems: it is difficult to wear them on the body, it is difficult to control them and it is difficult to transmit feedback back to the nerves, so that the user will regain feeling in his hand and fingers.
After some deliberation, Normak decided to get a new kind of prosthesis: one that becomes a part of the body for all intents and purposes. The robotic prosthesis was attached to his body through a process of osseo-integration: a metal implant - usually made of titanium - was inserted into the bone, and the bone cells were encouraged to migrate into the perforated metal and fill it with healthy bone tissue. In other words, the bone and the metal - the living and the inanimate - naturally integrated together[4].
The prosthesis Normak received not only integrated with the bone, but also with the nerves and muscles. Smart electrodes were matched to the appropriate nerves, and sophisticated algorithms translated the messages into instructions to be sent to the robotic arm, palm and fingers. The information flowed in both directions: when the robotic fingers touched the apple, for example, an electrical signal was immediately transmitted back to the sensors located around the nerves. The nerves sent the information back to the brain, so Normac could also enjoy a real sense of touch[5].
"I usually say that with a traditional sleeve prosthesis, you wear the prosthesis - it's a medical device. But with osseointegration, the medical device becomes part of you. You don't feel like you're wearing the prosthesis. Instead, she is a part of you.” said.
The story of Rickard Normack teaches us several lessons. First, it clarifies that we cannot automatically treat replacement organs as if they were purely biological. Similar to the synthetic polymer sheet on which Anthony Atla implanted Luke's bladder cells, Normac's arm also became a combination of the biological alongside substances that do not exist naturally in the body. We automatically shy away from such combinations - which many see as monstrous and unnatural - but it is impossible to deny the enormous benefit they bring to their owners.
The second important lesson is that prostheses do not have to continue to look like the original limb. Videos showing Normak's prosthesis reveal the point of its connection with the arm - a sight that provokes penetration. But again, even here, precisely the willingness to ignore the original shape of the limb, can help the recipient of the prosthesis.
We see here the continuation of a movement that started in the late seventies, when Van Phillips - a young student - had an accident that ended in the amputation of his leg below the knee. The prostheses fitted to him were so unsatisfactory that he switched to biomedical engineering and developed prostheses that were more useful than representational. This was the time when materials engineering leaped forward, and strong and light materials from the aviation industry began to find their way into prostheses as well. Philips developed the Flex-Foot, whose spiritual descendants allow runners in the Paralympics to reach speeds that rival those of non-disabled runners[6]. These prostheses don't look like legs, but they give the user mild superpowers.
Nowadays people seem to be less ashamed of their replacement organs. You can find pictures online of diamond encrusted, bright pink prosthetic arms and legs with wolverine claws, and plenty of other cyberpunk inventions. Designers are just beginning to explore the realms of possible beauty and form of replacement organs, and it will be fascinating to see where they take us.
This second lesson also has an important meaning for internal organs: we don't have to recreate them exactly the way they originally existed.
Take, for example, the pancreas. This complex organ is able to sense the levels of glucose - sugar - in the blood, and secrete insulin that will lower the blood sugar level. Biomedical engineers have labored for many years to create an artificial pancreas that can perform all these tasks. In fact, they are still trying. But it is also possible in another way: a modular artificial pancreas, that is, one that is broken down into different parts. A glucose sensor is attached to the skin at all times, and checks blood sugar levels. The information is transferred to an artificial intelligence that decides whether an insulin injection is necessary and determines the required doses. Last but not least, a pump pumps the insulin into the body through a tiny needle.
Each of these parts is located in a different place on the body. This is not a "pancreas" as we know it, but when they work together - they take the place of the biological pancreas. The final goal is important, not the way to achieve it.
This lesson also opens a window for us to strange and magnificent imaginations of the future of the replacement organs. Perhaps, instead of one and only one heart, we can place several artificial pumps in several places in the body, which together will fulfill the same function of the heart and circulate the blood throughout the body? Maybe the solution for a replacement liver is not one biological liver, but a series of filters that neutralize toxins and break down pollutants?
Maybe. maybe not. It's just important to understand that in the field of tissue and organ engineering, we don't have to be limited to 'the existing product'.
The third lesson from Normak's story is that today's technologies have reached a level where they can interface with the brain and the nerves. This has great implications for the future, which we will touch on in the last part of the article. In the meantime, we will return to the ground of reality and examine another type of organ alternatives: biological alternatives.
Let's talk numbers for a moment. In the United States alone, 106,075 people are currently waiting for an organ transplant. Some of them will never get the organs they need, because living donors provide only 6,000 organs a year, on average. An average of 17 people die every day while waiting for an organ transplant. Every nine minutes, a new person is added to the waiting list. In short, the statistics are not in favor of those waiting to receive an organ from the animal.
There are currently three main methods for creating replacement organs: decellularization, creating organoids, and XNUMXD printing. Each of them has its advantages and disadvantages, but one thing they all have in common: they still have a lot of room for improvement.
Let's start with decellularization.
We tend to think that the body is composed of cells - which is true, but partially. In fact, the cells secrete around themselves a tissue known as the "extracellular matrix", and within it they sit. The matrix supports them, stabilizes them and even 'communicates' with them and gives them chemical instructions that other cells secrete into it. Without the extracellular matrix, the cells in our body would not be able to function or survive.
Methods of decellularization - removal of cells - rely on the extracellular matrix as the basis of the tissue. In the first step, the tissue is washed and cleaned of all cells. What is left behind is the clean matrix: a structure that looks like the original organ, but devoid of color and life. The reason this empty structure is so valuable is that it contains all the proteins and growth factors—all the chemical instructions—that new cells can rely on to repopulate the tissue. Not only that, but it is also shaped in exactly the right way: heart, liver, bone or any other organ.
The decellularization method is currently used in some cases, such as breast reconstruction. Matrices cleaned of their cells are implanted in the breasts, and very successfully attract the cells that make up the blood vessels in the body, so that they penetrate into the matrix and fill it with blood vessels. After that, cells that divide and develop into fat cells are also injected into the matrices[7].
Unfortunately, I am not aware of a case of replacing a complete and complex organ in a person, with a decellularized matrix. In one of the most advanced studies in pigs, they received the heart of another pig that had been cleaned of its cells. They managed to survive for three days, before the hearts were harvested for close examination under the microscope lens. Obviously for humans we are interested in longer term success[8].
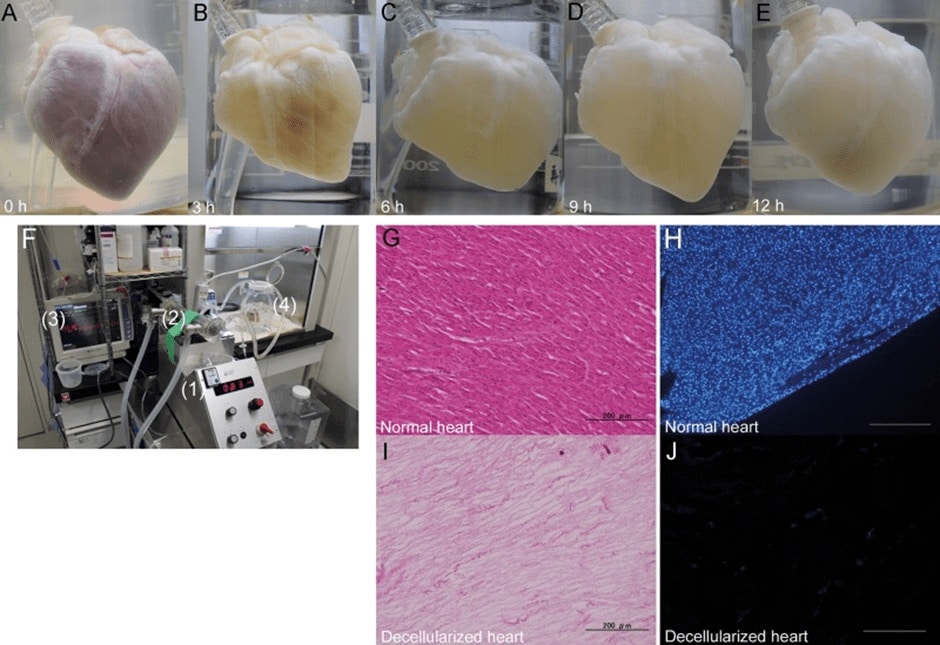
Another problem with decellularization is that the method still requires reliance on organs that come from humans. It is theoretically possible to use matrices of animal origin, but obviously these will not be as successful as human matrices.
organoids
In the middle of 2021, a strange news appeared in the international press: "mini-brains in the laboratory grew their own pairs of eyes". It's one of those tidbits you'd expect to see in science fiction, but it's decidedly contemporary. Those 'mini-brains' are the organoids.
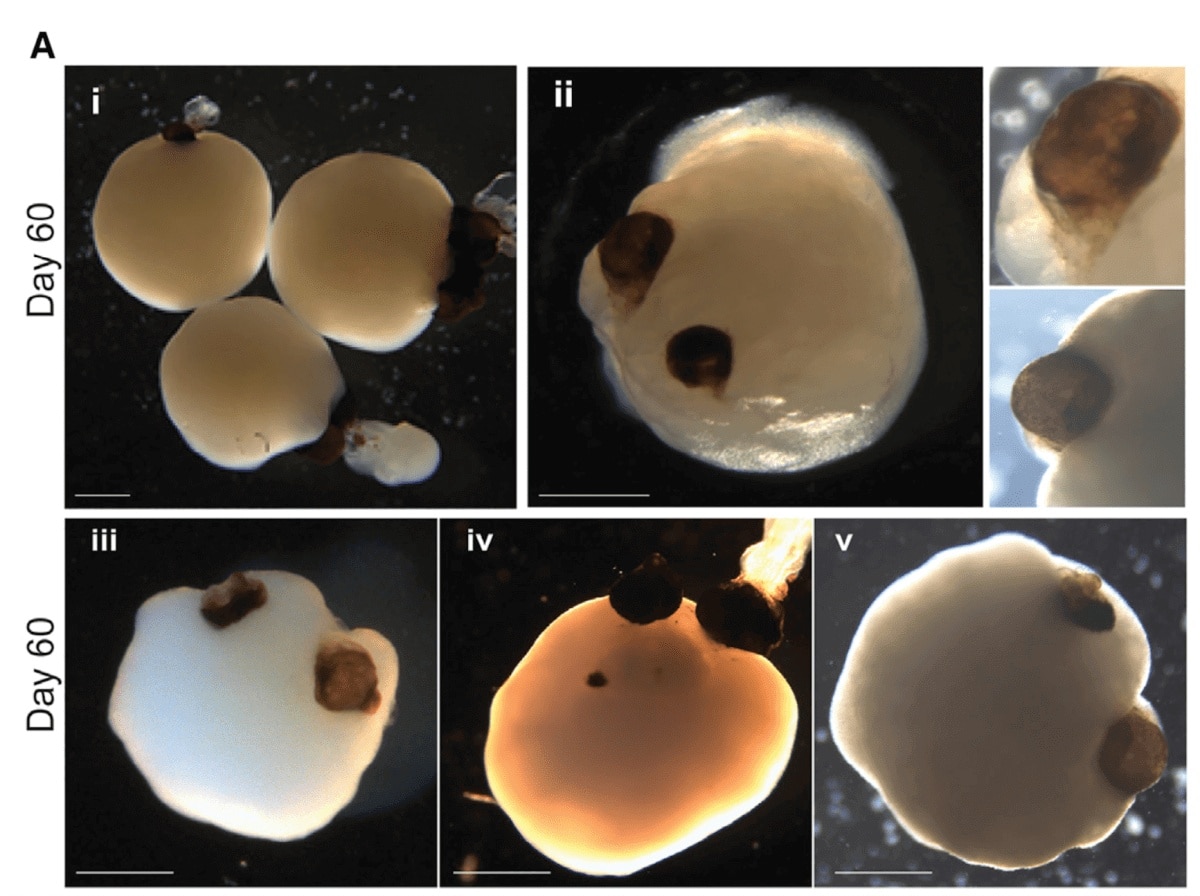
To explain where organoids come from, we first need to know the stem cells: a type of primitive cells capable of differentiating into many different types of body cells. The human embryo, in its earliest stages of development, is composed of such stem cells. These cells receive different instructions in the body of the fetus, and accordingly differentiate into different tissues: brain tissue, liver tissue, bone tissue and all the rest.
What will happen if we take stem cells, put them in a petri dish and give them instructions to create a certain tissue? They produced an "organoid" - a mini-tissue that mimics the tissues and organs of the human body.
In the same knowledge of mini-brains that grew new eyes, the organoids received instructions from the researchers to differentiate and create nerve cells and brain structures. Naturally, the growth continued to form the nerves that lead to the eyes, and the optic cups - basic structures that are supposed to grow the retina - appeared within thirty days and matured by the fiftieth day. This is also the estimated length of time for a similar development in the human embryo. The organoids also went on to develop lenses and corneal tissue[10].
Does this mean that we will soon be able to implant biological eyes, which will be developed on an organoid?
Unfortunately, that doesn't appear to be the case. The organoid is a mere imitation of the original organ. Although it is identical in its internal structure to the structure of the real organ, it is not suitable for transplantation or connection with a human body. There is also always the fear that the stem cells will get out of control in the transplanted body, and produce a deadly cancerous tumor. For these reasons, the organoids are not yet used to replace organs within the body. The most interesting use of them is precisely to replace organs outside the body: researchers are testing a variety of therapeutic substances on them, with the assumption that if these substances are harmful to the organoids, then they will also cause damage to the real organ inside the body.
This means that organoids are definitely used. As replacement organs outside the body, they help accelerate the pace of medical science progress. But in the clinical field, unfortunately, there is still no real progress.
Tissue printing
And so we finally arrive at the most promising and interesting method - or at least the one that gets the biggest and most frequent headlines in the newspapers. This is, of course, XNUMXD tissue printing.
The XNUMXD printing process usually begins with harvesting the patient's own cells. Doctors perform a small biopsy using a needle, or minimally invasive surgery. All this to obtain a small piece of tissue, from which the cells can be removed and grown outside the body. The cells spend the following days and weeks in bioreactors, where they enjoy an environment similar to that of the body, including temperature, oxygenation level, food - and even day-night cycles and physical activity, in some studies.
There are several different printing methods, but one of the most common is the one in which the cells are printed directly together with the matrix from which the tissue will be built. When there are enough cells in the bioreactors, they are mixed with the printing material - which is basically a preliminary version of the extracellular matrix. That matrix is pre-enriched with growth factors - that is, chemical instructions - that help the cells understand what they should do in that area. The printable matrix is often composed of materials such as gelatin and collagen, which do not harm the body or cells.
The cells and bio-ink are transferred to a XNUMXD printer, which injects them in the right areas. If you want to create a complex tissue - for example, a heart - then there will be several print heads, each of which will print different cells with a slightly different matrix for each type of cell. As a normal printer is able to print in several colors using several print heads or several different color cartridges, so too the XNUMXD printer prints different types of tissue, each in the right place in the organ.
The entire printing process should not take more than a few hours, and the final structure should be very similar to that of the desired organ. Theoretically, it can even be adjusted in size and shape, relying on information that comes from x-rays and scans of the patient's original organ.
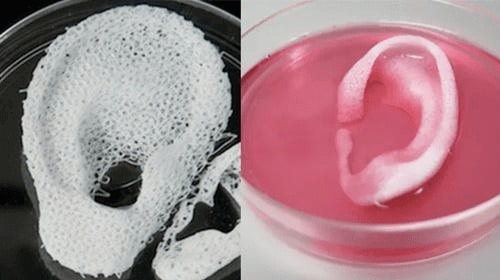
Only one problem remains: the entire impressive organ that was printed, begins to be destroyed during the printing process. The reason is that cells need oxygen and nutrients, and these cannot easily permeate through dense tissue. Therefore, there is a need for blood vessels that saturate the tissue with oxygen. The most advanced printers are supposed to print the blood vessels as well, but these still do not function easily or well, and it is necessary to connect them to existing blood vessels and actively flow oxygen through them. This means that as soon as the printed tissue reaches a certain thickness, the cells in its depth stop receiving oxygen - and begin to die.
What to do? Biting lips and transplants. They try to deliver as much oxygen as possible to the cells deep in the tissue to keep them alive, and transplant the tissue as soon as possible to let the body do what it knows how to do. The hope is that after the transplant, the existing blood vessels around the area will be sent out into the new tissue and flow oxygen and new blood into it. Emphasis on "hope", since this is a challenge that has not yet been resolved.
Either way, after implantation the artificial matrix begins to disintegrate and disintegrate, just as we want it to. It did its job, provided the cells with a foothold and the initial instructions they needed to stay alive - and now it is slowly being replaced by a new matrix that the cells secrete themselves.
This, in a nutshell, is the process of XNUMXD tissue printing. This is an almost futuristic procedure, which has already proven itself in many studies - but has not yet entered medical practice. She just isn't progressing far enough yet. The structures it creates are not stable enough, the cells in the depths of the tissue suffer from a lack of oxygen and food, and if we are honest - it is also very expensive. Ideally, cells that come from the patient's own body are used, and the entire process required to produce them, grow them and seed them using the printer, takes a lot of time and dedicated care.
I am used to talking about the various methods accepted today in the field of tissue engineering, and I am also used to the answer that is immediately thrown at me: so why not try?
Yes, XNUMXD printers are still not very efficient in printing tissues, but why not use them to print a basic kidney after all, implant in the body and hope for the best? Why not take organoids containing mini-brains, disassemble them and transplant them into the brains of Alzheimer's and Parkinson's patients, so that the nerve cells they contain will restore the lost brain structures and take the place of the dead cells? Why not decellularize scaffolds that come from animals, and just - well, try?
We got the answer to the question in the last decade, when an Italian surgeon named Paolo Macchiarini became "one of the most famous doctors in the world", according to the BBC. He rose to prominence thanks to a new procedure he developed to replace a trachea - windpipe - with tissue that has been emptied of cells and populated with stem cells. Over the course of three years, he performed the procedure on nine patients who had lost hope of living a healthy life without close assistance from the ventilator. The surgeries were widely and sympathetically covered by the media, but the results did not live up to the hype. Of the nine transplanted, seven died in the three years after the transplant, and one survived only after the artificial trachea implanted in his throat was removed[11].
In retrospect, it turned out that the experiments carried out by Macchiarini were tainted by negligence, and that the man developed a love-love relationship with the scientific community and the media, which allowed him to exaggerate with lies about the positive results of the experiments and analyses. Verbal love, by the way, because the surgeon also made the reporter fall in love with him, lied to her that he was divorced, and promised her a star-studded wedding, in which the Pope himself would marry the two and Elton John would serenade them.
A number of conclusions can be drawn from the episode. For example, don't lie in science. Another conclusion that scientists know very well is that every scientific field is much more complicated and complex than it appears from the outside, and that there are many more ways to fail than to succeed. This is especially true in medicine.
A third conclusion is that every experiment in medicine has rolling consequences, also on the public mindset and among the scientific community. Following the Macchiarini scandal, the entire scientific community was attacked with severe skepticism about tracheal transplant surgeries. When Dr. Eric Ganden set out to try to save a woman's life by replacing her trachea with a donor, his colleagues warned him not to even attempt to enter this minefield. He thought his job -
"It became unnecessary, so you basically close the lab. You can't justify doing experimental surgery... when you see something else that looks perfect. So you understand, wow, that they don't need you."
In the end, Ganden decided to perform the medical procedure, transplanting part of a donor's trachea into a woman who was no longer able to live with the damaged trachea she was gifted with. The surgery went smoothly, and today she got her life back. But it is quite possible that if not for the practice of Macchiarini - who in fact conducted irresponsible experiments on the backs of the patients - she and others would have been able to enjoy normal breathing much earlier. In medicine, as in science, there are no shortcuts.
All this does not mean that there is no need for bold experiments or the development of innovative and unusual techniques. But one should always maintain modesty and understand that most of the hidden is visible, and that any attempt to jump into the deep water will almost always lead to drowning. And in the worst case the result will not be the death of one person, but also damage to the entire field over many years. Such damage will ultimately result in delaying the time required until patients can receive tissues that will be extracted and implanted in safer ways.
In 1908, the first attempt at transplanting a whole head was made: the head of one dog was transferred to the neck of a second dog. The experiment failed and both dogs died, but that was just the beginning. The technology continued to develop, and in the seventies Robert White was able to perform the first head transplant in monkeys. The monkey whose head was transferred to another body managed to survive for eight days, while being able to move the facial muscles, and endowed with the sense of smell, taste and hearing. Similar experiments were also conducted in mice and rats, and in recent years also in human bodies.
These days there are already surgeons who promise that in the next decade they will perform a complete head replacement. When that happens, everything will change. We can, in practice, transfer souls from body to body. As long as any person has enough money, he can use it to acquire a new, young and fresh body. Or lightly used, and still - better than dying from cancer or another serious illness.
If the thought sounds shocking to you, you should remember that the immediate public reaction to the first heart transplants was that the doctors were "playing at being God" and having fun violating the laws of nature. It is also worth remembering that for the vast majority of people, the idea of a heart transplant or in vitro fertilization also seemed like science fiction, right up until the moment when these procedures were successfully tried, and then they became part of our normal way of life[12].
Still, it is impossible to ignore a big and real ethical question regarding head and brain transplants: is it fair to donate an entire body to save the life of a single person, while the same body contains a large number of other tissues that could have helped many others? One donor, after all, can donate his eyes, kidneys, heart, liver, skin and other organs. Or he can give one and only one body to one 'donor'.
I am convinced that this is a question that we will still have to deal with in the foreseeable future, but it will not bother us for many years. The reason, in a word, is automation. And in two words - Elon Musk.
Elon Musk founded the company Neuralink in 2016, with the aim of developing an interface that would connect to the brains of humans and allow them to communicate with machines - and machines to communicate directly with the brain. The company ran forward quickly, and had already managed to do a lot. or a little Depends on who you ask.
If you ask the general public, you will find people telling you with wide eyes that Neuerlink was able to read the brain waves of a pig using electrodes attached to its brain. They will report to you that the Neuralink monkeys can already play on the computer without moving the tip of their tail let alone their fingers, but through thought alone. The interface reads their brain activity and translates it into computer control. Indeed, miracles and wonders.
If you approach neurologists and ask them about Neuralink, you will be met with a knowing grin. Yes, the company has really succeeded in reading the brain activity of monkeys and pigs, they will tell you, and then casually add that these are things that scientists in their laboratories have already done twenty years ago. In other words, there is nothing new under the sun, except PR.
The truth is that they are both right. Neuralink is still far from innovating in the field of neuroscience, but here we are watching a company that actually manages to get up from scratch and reproduce experiments that were previously conducted in the most advanced laboratories in the world and rely on vast hidden knowledge: how to treat monkeys and pigs, how to insert electrodes, how to keep everyone alive, how to do signal processing and more and more. You could say that with the monkey she has almost finished reproducing what happens in the laboratories, and now her researchers have the necessary skill and experience to go further.
Two things particularly interest me about Neuralink, both of which could have a huge impact on our lives in the future. , and both are worth dwelling on for a moment.
The first is that Neuerlink intends - eventually, when its technology is advanced enough - to provide everyone with a way to directly control their own minds. Musk's vision is of a layer of electrodes that will be inserted into the biological brain in a simple way and without medical complications, and through which we can tell the brain what to do. There is no need to advance to - or nightmarish - science fiction stories that promise us advanced mind-reading abilities. Even if we can only control the secretion of neurotransmitters - serotonin, dopamine and others - then the world will change overnight.
Imagine a future world where you come home tired and exhausted from a hard day's work, but still yearn to write the book you've always dreamed of. With the push of a button, you instruct your brains to be more curious, more energetic, more ready to spill knowledge onto the keyboard. Or maybe, on another button, you allow yourself to open up more to your inner feelings, become more empathetic and connect more with your wife and children. A third button will suppress your hunger, or increase your ability to control your urges to help you diet.
How does such a world sound to you? dream? Nightmare? both?
In my opinion, the great thing about this vision is the choice it gives to every person. You will have to choose what is more or less important to you. You will have to decide how to divide the time, attention and love between all the tasks and beings that surround us. Musk wants, in fact, to give us a super-brain that we can use to make decisions about things that were previously largely subject to our environment and basic biology: emotions and moods.
And again - a dream or a nightmare? You decide. You probably won't have to make this decision in the next decade, but I would be surprised if in twenty years there aren't people who will already benefit from such a superior brain.
The second interesting point about Neuralink is that the company has developed, it claims, a robot capable of automatically performing the complicated operation of inserting the electrodes into the brain. According to the publications - which should be treated with great suspicion - the robot is currently capable of inserting almost two hundred electrodes per minute, using a thin needle and a hole it opens in the skull. Of course, at the end of the operation, he also nicely closes the hole with a kind of 'plug' the size of a half shekel coin, which also contains a transmitter through which the electrodes communicate with the environment[13].
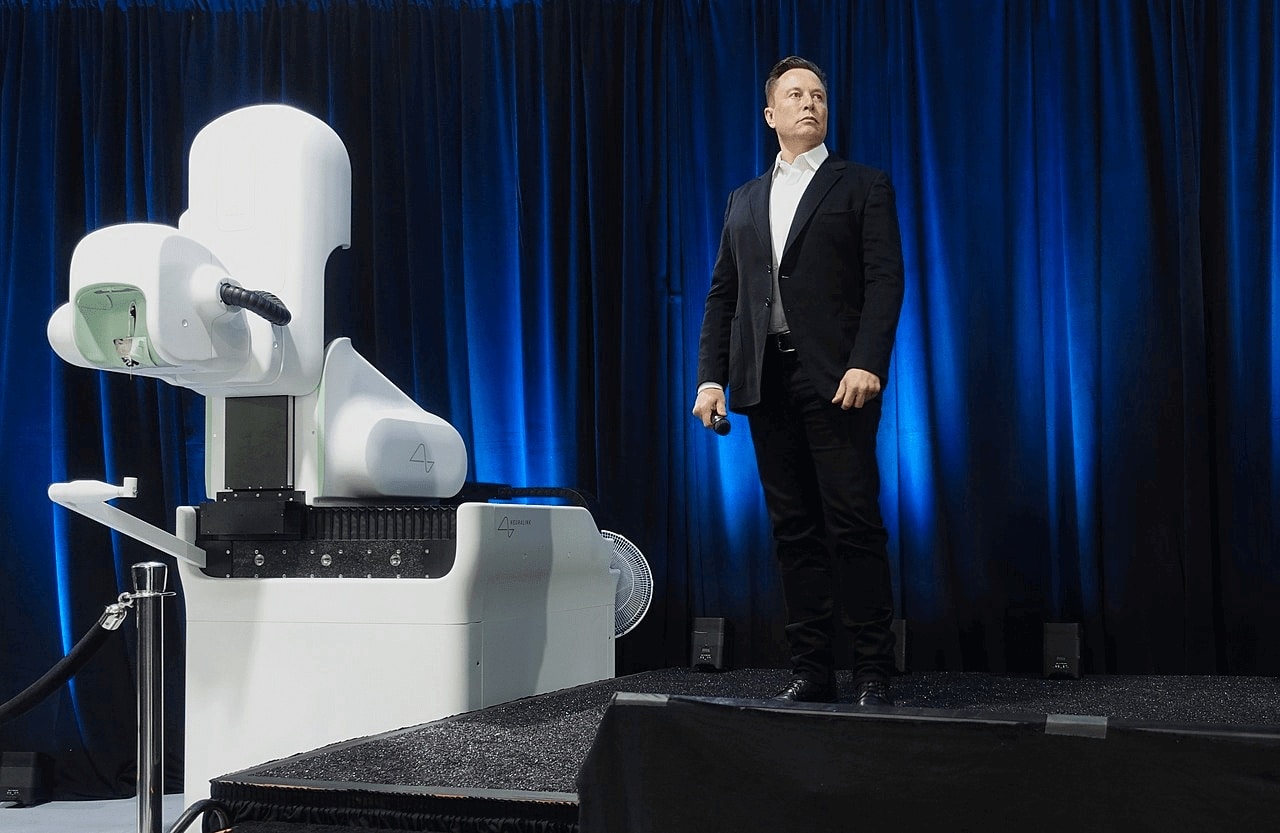
Many things can be said about Musk - not all of them are good - but he understands that the future will be shaped by a large number of different technologies that will integrate with each other. Sophisticated robots, for example, will be able to minimize the costs of implanting electrodes in the brain and the risk involved in such a procedure. Such robots do not exist, yet, but Musk already predicts their existence, and I agree with him. Robots with such a level of capabilities should reach realization in the next decade.
And now think about robots with a similar level of capabilities that will also work in laboratories and hospitals: robots that can take tissue samples from patients, grow the cells and take care of them in the laboratories, print the biological tissues - and finally also transplant them into the patient's body.
Is this future too strange for you? We will be more conservative: even if the entire role of the robots amounts to 'only' growing human tissues in the laboratory, it will still mean that the costs of replacing the tissues will decrease significantly. Automation - the ability to produce tissues automatically - for the most part - will ensure that even the poor can receive replacement tissues, as long as they live in a country with a functioning health and welfare system.
Make no mistake: none of this is going to happen in the coming years, and probably in the current decade we will still not be able to produce a variety of tissues for everyone. But for the fulfillment of such a great goal, which will jump us halfway to the promised eternal life, we can wait even two or three decades. And even if you can't really wait, well - there's no choice.
Biomedical engineers have been working for decades on the ability to replace tissues and even whole organs in the human body. There are methods with great potential for replacing tissues, the main one of which is printing the replacement tissues in XNUMXD before implanting them in the body. We also see a willingness on the part of the engineering and patient communities to 'broaden horizons' and test unusual spare parts for the body, such as an artificial pancreas that consists of three separate parts - sensors, artificial intelligence and an insulin injection pump. Research is progressing rapidly, but the transition to medical practice is slower, appropriately in areas where any mistake can cost human lives.
Artificial intelligence and robotics can help us speed up the pace of scientific research and actual application, but even then - there is no doubt that there is still a long way to go. Still, I am convinced that already in this century - and probably already in the coming decades - every person will be able to win tissues and organs that will replace the ones he grew up with. And as the same professor of medicine told me: when we can replace the failing heart or the failing liver, renew the skin and patch the brain with young nerve cells - then we can, in fact, stop aging and restore everyone's youth.
God willing - soon these days.
[1] https://www.nature.com/news/2006/060403/full/news060403-3.html
[2] https://biofabexplorer.cast.org/case-stories/meet-luke
[3] https://journals.lww.com/jpojournal/FullText/2014/04000/Socket_Pressure_and_Discomfort_in_Upper_Limb.7.aspx
[4] https://www.hss.edu/condition-list_osseointegration.asp
[5] https://www.healthline.com/health-news/future-prosthetics-might-be-this-mind-controlled-bionic-arm#How-the-technology-works-compared-with-conventional-prostheses
[6] https://qz.com/2141720/modern-prosthetics-go-beyond-bionic-limbs-and-into-the-brain/
[7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6928092/
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4892160/
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4892160/
[10] https://www.livescience.com/brain-organoid-optic-eyes.html
[11] https://www.bbc.com/news/magazine-37311038
[12] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6511668/
[13] https://en.wikipedia.org/wiki/Neuralink
More of the topic in Hayadan:
